When Superstorm Sandy slammed into the Northeast nearly two years ago, hospitals found themselves dealing with surges in patients, lost power supplies and employees who couldn’t get to work — problems that a new federal report finds they were not prepared to handle.
When Superstorm Sandy slammed into the Northeast nearly two years ago, hospitals found themselves dealing with surges in patients, lost power supplies and employees who couldn’t get to work — problems that a new federal report finds they were not prepared to handle.
The U.S. Department of Health and Human Service’s Inspector General Office released a study Wednesday on the emergency preparedness and response during the storm at 172 hospitals in the hardest-hit areas of New York, most of Connecticut and all of New Jersey.
The report, based on surveys of the hospitals and in-person visits to 10 of them, finds that 89 percent of them experienced “critical challenges,” such as electrical and communication failures or problems getting enough fuel or beds to meet their needs. The report did not list which hospitals had which problems, but several were reported at the time of the October 2012 storm.
The report finds that most of the hospitals were cited in the three years before the storm for deficiencies related to emergency preparedness and response. In many cases, the issues cited by accreditation organizations were exactly the same ones that caused problems during the storm.
The surveyors found that 47 hospitals were cited for problems with their utilities — including several that infrequently or incorrectly tested their backup generators.
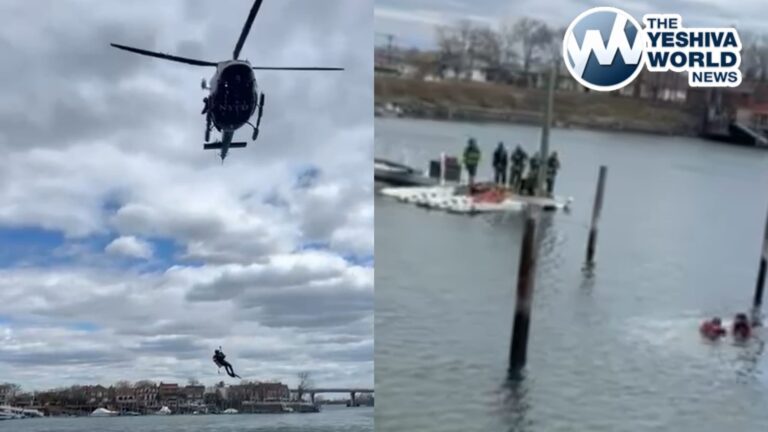
When the storm came, nearly half of the hospitals had electrical problems. And half of those that lost power had problems with backup generators. At New York City’s Bellevue Hospital Center, for instance, the fuel pumps remained in the basement and flooded. The hospital was ultimately evacuated.
Hospitals also said that some workers were not properly trained or experienced in working in no-power environments, meaning nurses had to be trained on the fly to do tasks such as counting IV drips manually rather than relying on technology to do it.
Researchers say that the problems did not lie solely with the hospitals. Some community emergency plans did not consider the needs of hospitals, for instance.
The researchers found that contributed to many problems, including worker shortages. In some communities, doctors and nurses were allowed to travel on roads closed because of the disaster, but other employees needed to keep the hospitals functioning — including maintenance and security staff — were not.
Nearly half the hospitals had surges in numbers of patients. Some received patients from the 12 hospitals that evacuated at least some of their patients. Others received patients from dialysis centers and methadone treatment centers that closed during the storm.
There was also an influx of patients with chronic conditions who needed important but relatively minor help, such as working power outlets so they could use oxygen tanks.
The hospitals said that some of those patients could have been served better by going to shelters, but that there were not enough of them in some cases, and in others those that were open were not publicized adequately. For patients in that category, providing help took staff members’ time, but the hospitals were not eligible for reimbursement from Medicaid or Medicare.
Hospitals also suffered financially during the storm as outpatient procedures and elective surgeries were canceled.
Irwin Redlener, director of the National Center for Disaster Preparedness at Columbia University and an adviser to New York Mayor Dill de Blasio on preparedness, said federal funding to help hospitals ready for disasters has been far less than needed.
“It’s so far down the priority list for administrators that nothing gets done,” he said.
He also said some hospital procedures have been updates since Sandy, but there is confusion about who should be coordinating plans and actions among hospitals. “You could imagine doing it in many different ways,” he said. “The worst thing is not doing it.”
(AP)