Eli Lilly will cut prices for some older insulins later this year and immediately give more patients access to a cap on the costs they pay to fill prescriptions.
The moves announced Wednesday promise critical relief to some people with diabetes who can face thousands of dollars in annual costs for insulin they need in order to live. Lilly’s changes also come as lawmakers and patient advocates pressure drugmakers to do something about soaring prices.
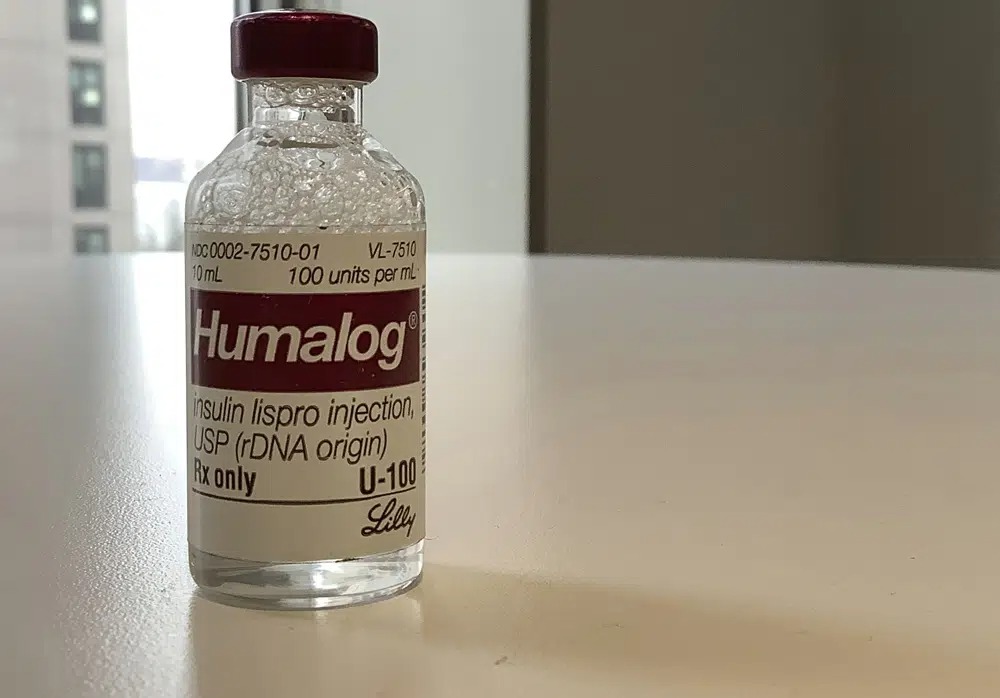
Lilly said it will cut the list prices for its most commonly prescribed insulin, Humalog, and for another insulin, Humulin, by 70% or more in the fourth quarter, which starts in October.
List prices are what a drugmaker initially sets for a product and what people who have no insurance or plans with high deductibles are sometimes stuck paying.
A Lilly spokeswoman said the current list price for a 10-milliliter vial of the fast-acting, mealtime insulin Humalog is $274.70. That will fall to $66.40.
Likewise, she said the same amount of Humulin currently lists at $148.70. That will change to $44.61.
Lilly CEO David Ricks said Wednesday that his company was making these changes to address issues that affect the price patients ultimately pay for its insulins.
He noted that discounts Lilly offers from its list prices often don’t reach patients through insurers or pharmacy benefit managers. High-deductible coverage can lead to big bills at the pharmacy counter, particularly at the start of the year when the deductibles renew.
“We know the current U.S. health care system has gaps,” he said. “This makes a tough disease like diabetes even harder to manage.”
Patient advocates have long called for insulin price cuts to help uninsured people who would not be affected by price caps tied to insurance coverage.
Lilly’s planned cuts “could actually provide some substantial price relief,” said Stacie Dusetzina, a health policy professor at Vanderbilt University who studies drug costs.
She noted that the moves likely won’t affect Lilly much financially because the insulins are older, and some already face competition.
Lilly also said Wednesday that it will cut the price of its authorized generic version of Humalog to $25 a vial starting in May.
Lilly also is launching in April a biosimilar insulin to compete with Sanofi’s Lantus.
Ricks said that it will take time for insurers and the pharmacy system to implement its price cuts, so the drugmaker will immediately cap monthly out-of-pocket costs at $35 for people who are not covered by Medicare’s prescription drug program.
The drugmaker said the cap applies to people with commercial coverage and at most retail pharmacies.
Lilly said people without insurance can find savings cards to receive insulin for the same amount at its InsulinAffordability.com website.
The federal government in January started applying that cap to patients with coverage through its Medicare program for people age 65 and older or those who have certain disabilities or illnesses.
President Joe Biden brought up that cost cap during his annual State of the Union address last month. He called for insulin costs for everyone to be capped at $35.
Biden said in a statement Wednesday that Lilly responded to his call.
“It’s a big deal, and it’s time for other manufacturers to follow,” Biden said.
He also noted that Americans “for far too long” have faced much higher drug costs than people in other countries.
Aside from Eli Lilly and the French drugmaker Sanofi, other insulin makers include the Danish pharmaceutical company Novo Nordisk.
Representatives for both Sanofi and Novo Nordisk said their companies offer several programs that limit costs for people with and without coverage.
Insulin is made by the pancreas and used by the body to convert food into energy. People who have diabetes don’t produce enough insulin.
People with Type 1 diabetes must take insulin every day to survive. More than 8 million Americans use insulin, according to the American Diabetes Association.
Research has shown that prices for insulin have more than tripled in the last two decades. Pressure is growing on drugmakers to help patients.
The state of California has said it plans to explore making its own cheaper insulin. Drugmakers also may face competition from companies like the nonprofit Civica, which plans to produce three insulins at a recommended price of no more than $30 a vial, a spokeswoman said.
Drugmakers may be seeing “the writing on the wall that high prices can’t persist forever,” said Larry Levitt, an executive vice president with the nonprofit Kaiser Family Foundation, which studies health care.
“Lilly is trying to get out ahead of the issue and look to the public like the good guy,” Levitt said, adding that there’s nothing stopping Lilly from raising prices again in the future.
Lilly officials said Wednesday that they have not raised the price of any of their insulins since 2017.
Ricks, the Lilly CEO, said the drugmaker made the changes announced Wednesday “because it’s time and it’s the right thing to do.”
Indianapolis-based Eli Lilly and Co. became the first company to commercialize insulin in 1923, two years after University of Toronto scientists discovered it. The drugmaker then built its reputation around producing insulin even as it branched into cancer treatments, antipsychotics and other drugs.
Humulin and Humalog and its authorized generic brought in a total of more than $3 billion in revenue for Lilly last year. They rang up more than $3.5 billion the year before that.
“These are treatments that have had a really long and successful life and should be less costly to patients,” Dusetzina said.
(AP)