As more doctors prescribe Pfizer’s powerful COVID-19 pill, new questions are emerging about its performance, including why a small number of patients appear to relapse after taking the drug.
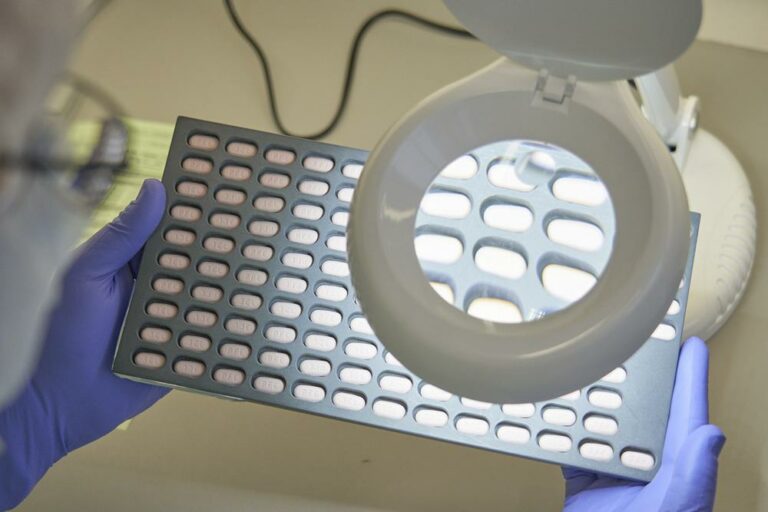
Paxlovid has become the go-to option against COVID-19 because of its at-home convenience and impressive results in heading off severe disease. The U.S. government has spent more than $10 billion to purchase enough pills to treat 20 million people.
But experts say there is still much to be learned about the drug, which was authorized in December for adults at high risk of severe COVID-19 based on a study in which 1,000 adults received the medication.
WHY DO SOME PATIENTS SEEM TO RELAPSE?
Doctors have started reporting rare cases of patients whose symptoms return several days after completing Paxlovid’s five-day regimen of pills. That’s prompted questions about whether those patients are still contagious and should receive a second course of Paxlovid.
Last week, the Food and Drug Administration weighed in. It advised against a second round because there’s little risk of severe disease or hospitalization among patients who relapse.
Dr. Michael Charness reported last month on a 71-year-old vaccinated patient who saw his symptoms subside but then return, along with a spike in virus levels nine days into his illness.
Charness says Paxlovid remains a highly effective drug, but he wonders if it might be less potent against the current omicron variant. The $500 drug treatment was tested and OK’d based on its performance against the delta version of the coronavirus.
“The ability to clear the virus after it’s suppressed may be different from omicron to delta, especially for vaccinated people,” said Charness, who works for Boston’s VA health system.
Could some people just be susceptible to a relapse? Both the FDA and Pfizer point out that 1% to 2% of people in Pfizer’s original study saw their virus levels rebound after 10 days. The rate was about the same among people taking the drug or dummy pills, “so it is unclear at this point that this is related to drug treatment,” the FDA stated.
Some experts point to another possibility: The Paxlovid dose isn’t strong enough to fully suppress the virus. Andy Pekosz of Johns Hopkins University worries that could spur mutations that are resistant to the drug.
“We should really make sure we’re dosing Paxlovid appropriately because I would hate to lose it right now,” said Pekosz, a virologist. “This is one of the essential tools we have to help us turn the corner on the pandemic.”
HOW WELL DOES PAXLOVID WORK IN VACCINATED PEOPLE?
Pfizer tested Paxlovid in the highest-risk patients: unvaccinated adults with no prior COVID-19 infection and other health problems, such as heart disease and diabetes. The drug reduced their risk of hospitalization and death from 7% to 1%.
But that doesn’t reflect the vast majority of Americans today, where 89% of adults have had at least one shot. And roughly 60% of Americans have been infected with the virus at some point.
“That’s the population I care about in 2022 because that’s who we’re seeing — vaccinated people with COVID — so do they benefit?” asked Dr. David Boulware, a University of Minnesota researcher and physician.
There’s no clear answer yet for vaccinated Americans, who already have a hospitalization rate far below 1%.
That may come from a large, ongoing Pfizer study that includes high-risk vaccinated people. No results have been published; the study is expected to wrap up in the fall.
Pfizer said last year that initial results showed Paxlovid failed to meet the study’s goals of significantly resolving symptoms and reducing hospitalizations. It recently stopped enrolling anyone who’s received a vaccination or booster in the past year, a change Boulware says suggests those patients aren’t benefitting.
At a minimum, the preliminary data should be released to federal officials, Boulware said. “If the U.S. government is spending billions of dollars on this medicine, what’s the obligation to release that data so that they can formulate a good policy?”
CAN PAXLOVID BE USED TO HELP PREVENT COVID-19 INFECTION?
Pfizer recently reported that proactively giving Paxlovid to family members of people infected with COVID-19 didn’t significantly reduce their chances of catching it. But that’s not the end of the story. Pfizer is studying several other potential benefits of early use, including whether Paxlovid reduces the length and severity of COVID-19 among households.
“It’s a high bar to protect against infection but I’d love to see data on how Paxlovid did against severe disease because it may be more effective there,” said Pekosz.
(AP)










One Response
I could not find a single study on Hydroxychloroquine that was properly conducted;
Every single study that failed, has either omitted the absolutely necessary Zinc, or was conducted late-stage (after a week after symptoms) or BOTH problems!
(Paxlovid too needs to be taken within 5 days of symptoms.
Go ahead, be my guest and try to find a single failed study that was properly performed.
Note:
I did find a few studies that were conducted properly (correct doses of HCQ, and Zinc, and done early stage)
and they had excellent results!
(Approximately as good as Paxlovid’s results.)
We live in a world of blinded lemmings…
p.s.
HCQ is not for anybody with a heart condition.
I guess for them Paxlovid is really the best option.
Anyway, both require a doctor/prescription. (As does Ivermectin, which also requires combining with Zinc.)